There is an increased demand for serology testing for SARS-CoV-2 to identify people who have been exposed to the virus and who may have developed an immune response. However, there are questions about which viral protein to use as an antigen for serology testing. Some diagnostic developers are not able to be definitive because this is a new virus, although based on the information we have, the viral protein is perceived as the obvious candidate.1
The Coronavirus

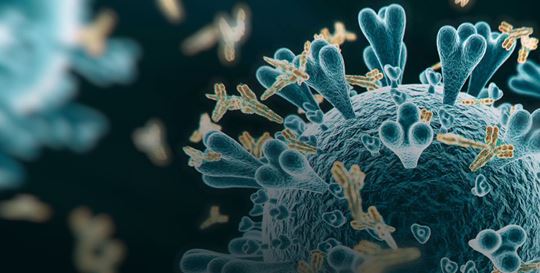
A coronavirus contains four structural proteins, including spike (S), envelope (E), membrane (M), and nucleocapsid (N) proteins.
The coronavirus gets its name from the spike like protrusions that look like a crown. These viruses use the spike protein to bind to proteins on the host cell to gain entry. In the case of SARS-CoV-2, the spike proteins bind angiotensin-converting enzyme 2 (ACE2 receptor) on human cells with high affinity.2
The Value of the Spike Protein
Though the coronavirus uses many different proteins to replicate and invade cells, the spike protein is the major surface protein that it uses to bind to a receptor. After the spike protein binds to the human cell receptor, the viral membrane fuses with the human cell membrane, allowing the genome of the virus to enter human cells and begin infection.3
Studies have also shown that the S protein plays the most important roles in viral attachment, fusion and entry, and it serves as a target for development of antibodies, entry inhibitors and vaccines.4–10
The coronavirus spike protein mediates entry into host cells by attaching to a receptor on respiratory cells called angiotensin-converting enzyme 2, or ACE2,11 the existence of antibodies against it may suggest neutralization of SARS-CoV-2 infection.
To assess this, a study performed a pseudovirus particle-based neutralization assay and found that there was a significantly positive correlation in the neutralizing antibody titers between pseudovirus and SARS-CoV-2. The study demonstrates that most recently discharged patients had strong humoral immunity to SARS-CoV-2.12
Research also shows that the S protein undergoes dramatic conformational changes to expose the RBD and key residues for receptor binding to enter the host cell. Given the critical role of the RBD in initiating invasion of SARS-CoV-2 into host cells, it becomes a vulnerable target for neutralizing antibodies.13

 English
English